I’ve had a number of conversations of late with self-insured employers about their workers’ comp “savings” reports; one thing that keeps coming up is how- and why – vendors ‘game’ the numbers.
(this post is a follow up to a post I did seven years ago…)
Perhaps the greatest variation is in bill review “savings” – and the fees attached to those “savings”.
Bill review savings are reported as a percentage below the applicable fee schedule or, in states without fee schedules, usual and customary rates or billed charges (depending on the vendor and state). Savings are also attributed to application of state rules, for example a denial of an assistant surgeon’s fee or physical therapy 59 modifier. These savings don’t generate additional fees for the vendor as they arise from mere application of state regs and fees.
One would think this is an objective result, and therefore there should be little variation among and between vendors, and in an ideal world, one would be right.
However, there is almost always a bit of judgment involved in determining what the ‘right’ fee schedule amount is and what state rules apply. The complexities are many, and the justifications, while often thin, are given to payers unequipped to refute the vendor’s statements.
Then there is the gamesmanship where savings that should be attributed to fee schedule or application of state rules are put in a different bucket, a bucket that just happens to generate additional fees for the vendor.
Let’s look at the ‘why’ vendor BR savings vary.
Simply put, follow the money.
Most bill review services these days are priced on a flat charge per line or per bill; Most BR vendors also charge for additional ‘value-added’ services on a percentage of savings basis – typically 25% of savings delivered on top of fee schedule/UCR cuts. That’s where the…variation usually lies.
The financial motivation is obvious; the vendor gets the same fee for processing a bill whether they deliver $1 or $1000 in BR savings, but their compensation for ‘value-added’ services is based on the savings that are delivered – the higher the ‘savings’, the greater the fees for the vendor.
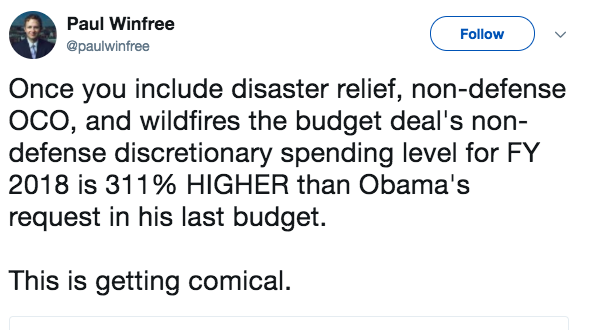
Therein lies one explanation – perhaps the most significant one – for the wide variation in BR savings percentages. In my consulting practice I’ve had access to reports from several of the larger BR vendors, and the variation can be as much as 300 percent from vendor to vendor. Yes, you read that right – one vendor’s bill review “savings” in a state can be three times higher than another’s.
Almost always the vendor with the lower FS savings delivers great results from ‘nurse review’, ‘complex bill review’, ‘coding edits’, ‘unbundling and upcoding review’, or whatever they call it – suffice it to say that the savings delivered from these ‘extra, value-added’ services – when added to the ‘standard’ bill review reductions – are usually only a bit higher than other vendors who don’t have all those extra, value-added add-ons.
That’s not to say that some savings can – and should – be derived from careful and professional review of bills – coding and clinical reviews are often helpful.
How can you protect yourself?
- Ask competing vendors to reprice a set of bills and provide savings numbers in aggregate and for each bill. Compare reductions from application of FS and state rules from the vendors, and on individual bills.
- Where there’s wide variation, ask the vendors for an explanation, and don’t accept mumbo jumbo BS.
- Make very sure your vendor knows you are holding them to the same standard they used in repricing your sample bill.
- Ask your colleagues if you can see their savings reports, and compare the savings allocations to your reports.
- Ask your broker, consultant, or adviser for their views, and get them to share de-identified client savings reports with you.
What does this mean for you?
The bad actors are known to many – make very sure you know who they are.