When Single Payer becomes the law of the land, Medicaid will be the foundation.
We’ve looked at the current push for Medicare for All, the factors that I believe will drive us to some form of single payer, and posted a primer on Medicaid.
Here’s why it’s going to be Medicaid for All.
- Medicaid for All will spread the cost of universal coverage across states, reducing federal financing requirements.
Medicaid is a state AND federal program; States provide a lot of the funding for Medicaid; on average the Feds contribute 63% and states 37%. This is critical, as Congress will want to spread the cost of a Single Payer solution and there’s no better way to do this than require states to pony up big dollars [State contributions vary based on a state’s average personal income relative to the national average; states with lower average personal incomes get more federal dollars.] - Medicaid is already built to cover everyone.
Medicare covers people of all ages, Medicare is very much elder-care focused.
Adapting Medicare to handle everyone from newborns to elderly, maternity care to pediatrics will be difficult, time-consuming, and expensive. Medicaid does all this and more – today. - Generally, Medicaid is less expensive than other “systems”.
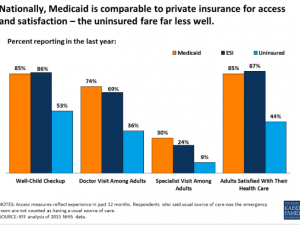
This is due to much lower provider payment and significantly lower administrative costs. Yes, this means providers are going to be paid less. - Medicaid member satisfaction is pretty good; access to care is not much of an issue.
- Medicaid-based Exchange programs are much more successful in the Exchanges than commercially-based plans.
The Centenes et al [Medicaid-based plans] understand the demographics of the uninsured, have lower medical costs, and already have provider networks, customer relations operations, workflows and processes set up and operational. At the end of the day, lower cost wins – and their costs are lower. - Medicaid is a simple, fully-integrated healthplan.
Medicare’s alphabet-soup of Parts A B C and D is confusing and convoluted, with different payers often covering the same individual. This increases administrative costs, member hassles, and decreases quality of care (co-ordinating pharmacy and medical care between different payers is problematic at best. - Managed Medicaid plans are working.
These plans currently exist in most states, and many have been able to deliver excellent care at lower costs through innovation and very tight focus on outcomes. One example is using paramedics to deliver care. [disclosure – I sit on the board of Commonwealth Care Alliance, a Massachusetts healthplan that serves dual-eligible members]
Tomorrow I speculate on how Medicaid for All will integrate with Medicare and employer-based coverage.
What does this mean for you?
Better care, lower costs, while a big impact on pharma, device companies, healthcare systems, and healthcare providers.



Joe,
Medicaid eligibility is based on how much money you have in the bank. Last year, when I was diagnosed with ESRD, I applied for both Medicare and Medicaid. I got Medicare because of the ESRD, and had Medicaid for four months, but lost it because I had gotten money from a program we put my mother’s assets into before she died. After she died, my brother and I each received a check in the same amount from that program. This was the amount of money we paid to purchase property in Florida so that the government could not get it and she could go into a nursing home. If you are advocating Medicaid for All, wouldn’t that mean that all Americans would have to have only $2,000 or less in the bank? If Medicaid is an income-based program, doesn’t it make sense to go to Medicare for All because there is no income requirement?
Good morning Richard – thanks for the question.
I would envision income requirements could be used to establish individual contribution levels (premiums), so people would have to contribute to their coverage at levels commensurate with their income. This is similar to how the ACA works now.
What a terribly sad day that will be. One of the greatest healthcare (HEALTH) systems in the world will be subpar as many other countries. We are already seeing this downward spiral in unreasonable wait times for appointments, MDs exiting healthcare in droves, projected critical nursing shortages, and necessary tests being denied due to unreasonable policies that have taken out the human factor. This is just the beginning.
Ask any Medicare patient how great their healthcare is! I doubt you’ll get many positive answers. (More like what DO they cover??!)
All in the name of controlling costs? Well, you get what you pay for right? Why does anyone think this will be any different!!??
Respectfully agree to disagree-
Susan
Hello Susan and thanks for the comment.
Couple questions – all the data I’ve seen indicates patient satisfaction with Medicare is significantly higher than the same metrics with commercial plans. What data do you have that supports your assertion re Medicare’s low patient satisfaction?
btw, the same is generally true with Medicaid.
source – https://www.ahrq.gov/sites/default/files/publications2/files/cahps-database-2017-hp-chartbook_0.pdf
Second, when you look at US healthcare outcomes, they are notably below other developed countries. Yet we pay more than twice as much for this poor quality care. https://www.joepaduda.com/2018/08/16/u-s-healthcare-vs-the-world-in-one-chart/
Do you have data supporting your assertion about the quality of our healthcare system?
Joe- Instead – I’m going to say look at Massachusetts. The previously richest state in the country is in a serious MESS. Universal health Care model right there. How can you say (if Romney couldn’t) that Universal Health Care works.
https://www.bostonglobe.com/metro/2016/03/22/even-with-health-insurance-massachusetts-residents-often-can-afford-care/TsjPf8tPuVmRoUfMUM3PhM/story.html
Disguise it anyway you want. Medicaid, Medicare –it will not be the same if it’s for all- so you can’t compare it to today’s model. We could never sustain it like today. So it’s not apples to apples
with any data you pull. We barely can afford to maintain it now.
And again, who is going to provide the care? Or should I say how long before the major shortage shows up? The job is hard enough, do you think the calling is going to be enough in the long run? America has gotten used to getting paid high wages for long grueling schooling. How many are going to pay that type of debt just to be overworked, underpaid and controlled by the government and fear of constant suits?
Yes, countries like Denmark have healthier health Care system (not better health care -novel technologies)). Also do you know how much of their income they give to the government? Way more than the US.
Denmark is also much smaller than the US. We also have a much larger population that does not contribute. So how is that comparable? I can compile data pro healthcare, but I can compile data against.
To me however, it’s fairly common sense to just looking at the mess the ACA has already created.
And we are barely in yet…. That days it all.
Hello Susan.
Clearly you have your views and data and facts will not sway them. The reality is Denmark and other OECD countries deliver far better care at much lower costs.
What you don’t seem to understand is you are paying – directly, thru lower wages, and thru taxes- for a healthcare system that is far too expensive.
If you want to keep this system, fine. Just don’t complain about your taxes or low wages. If you want your more and more of your dollars to go to pharma, providers, and facilities, that’s the decision you are making.
Joe’s favored plan is what 1/3 of all Californians are on. It’s a complete and utter disaster! Not many providers take the plan because it pays horribly. It’s not even worth spending the time to do the billing. That’s one of the reasons why so many patients in CA end of being treated at the ER for basic needs. But we all remember the promises, right??? You can keep your plan AND you can keep your doctor.
Joe is also OK with providers taking another 11-13% salary cut even though many of us make 30% less than we did in the 90s. Should we consider reducing the massive, ever-expanding administrative and regulatory overhead that has never been proven to improve care?? What about directing care toward cost-effective providers and centers? The truth is that if providers are cut further, the shortage of doctors will worsen. It won’t be worth it to go into medicine anymore. Why go into HUGE debt and spend over 10 years in training when you can blog or be a middleman consultant and net far more money???
Always good to hear from you IPT of CA.
You make a couple of statements that aren’t supported by facts; when did I say Medicaid was my “favored plan?”
You infer that Medicaid is why “so many patients in CA end of being treated at the ER for basic needs.” Source please?
Lastly, I find your claim that bloggers “net far more money” than physicians humorous indeed. Source please?
Happy to engage in a fact-based discussion of the merits and challenges inherent in a Medicare- or Medicaid-based system.
Here’s are some facts…. The state of CA is in DEBT hundreds of millions of dollars to the County of San Diego for the failed MediCal system. Billions when you include all the other counties. In a sense, the state is a deadbeat payer. And now the hospitals are all closing down their mental health units because they cannot afford to run on what MediCal pays, which is next to nothing. You see, sometimes when you give away too many freebies, many more suffer. Two community hospitals in our area have closed entirely. Why? They were overrun with very low-paying MediCal patients. So…it’s not surprising that our care would be measured as poor. Our system IS largely a MediCal system OR no care available at all!
Some would call what we have in CA failed redistribution scheme. It’s not the evil doctors’ fault that we have so many poor and homeless people in CA. Any plan blaming doctors for these problems or sticking it to them is not going to fly.
Agree with comment from Susan (above). You largely get what you pay for. Patients don’t get much with MediCal. This is largely our healthcare system in CA because 1/3 of patients are on it. We also have a WC system that allows providers to be paid at less than 50% of the fee schedule. Joe, many believe this is because of greed, as well as failed leadership that has not taken corrective action.
IPT of CA – citations please.
In the absence of reliable citations, I find your assertions lack credibility.
The reality is ALL research indicates US healthcare costs so much primarily due to higher prices paid for services – pharma, facilities, providers, devices, surgery. That’s the issue. I’ve reported on this dozens of times here.
Re your comment that “you get what you pay for”, that is unsupported by any citations or facts. In fact, about a third of US healthcare spend is for care that is dangerous or unlikely to benefit the patient. See https://khn.org/morning-breakout/iom-report/.
Re your insertion of non-germane comments on workers’ comp, that is a red herring.
Forgot to give you my sources:
Tri City Hospital- just closed mental health unit
Palomar Hospital- closing mental health unit
Fallbrook Community Hospital- closed for business
San Clemente Community Hospital- closed for business
4 hospitals going down in a very short period of time, largely because they have been overrun by MediCal!
IPT of CA –
Sorry, those aren’t sources – please prvide cite re reason for their demise. All research indicates these facilities’ closures were not due to Medical, but for many reasons.
You attribute these closures to MediCal – fact is small hospitals are going out of business nationally for a host of reasons. For many, increased Medicaid reimbursement due to higher enrollment in Medicaid has been a boon, as many of their now-insured patients were previously uninsured.
Other factors include:
– global capitation arrangements
– requirement for certifications for specific types of care
– loss of profitable specialty care to large hospitals
– lack of affiliation with hospital systems means operating costs are higher
– significant reduction in DSH payments
Fallbrook closed 4 years ago – just after ACA was fully implemented.
http://www.sandiegouniontribune.com/news/health/sdut-fallbrook-hospital-challenges-2014oct11-story.html
San Clemente closed over two years ago.
http://lariatnews.com/news/low-inpatient-numbers-causes-hospital-closure/
And neither was attributed to MediCal reimbursement, rather declining census and operating costs.
What you’re missing here is MediCal costs money, which means taxes. You can either pay providers more, or pay less in taxes. And no, the “middlemen” aren’t a factor – this is about MediCal and providers.
If we are to have a balanced, facts-based discussion, please post my prior comment regarding how CA owes the Counties billions of dollars in overdue MediCal payments. They owe the County of San Diego hundreds of millions but are not paying. The state appears to be a deadbeat payer. No wonder so many people think big government programs don’t work. They are bankrupting local municipalities with their failed promises!
it has been posted. If you want a fact-based discussion, please use facts, supported by credible cites. You have yet to provide any.
Well I do agree Joe I think this may be where things are heading. I have mixed emotions over it. In AZ AHCCCS (Medicare) is not the easiest to deal with. Too many rules and policies that make it challenging for providers to get paid. Once we do get paid we average just slightly higher than what most private commercial plans pay us but less than Medicare. I do not think providers can get hit any harder and be asked to take even less. I am no fan of the private commercial payers either as I have stated in a previous post on this topic. Do we want Wall Street or government bureaucrats managing our healthcare? One inefficient with too many cumbersome regulations and the other operating with greed and profits in mind. Neither sounds good to me. Why not figure out a hybrid system that is based on outcomes and great care/customer service, disease prevention/wellness model and pay providers accordingly. I believe you will see better outcomes in time.
My perspective is unique as I have experienced both the Canadian system as both a provider and patient. And, the US system of buying insurance for our employees, being a patient and provider. I can tell you based on my 25 yrs experience here in the states the big commercials are not friends of patients or providers but they sure know how to toe the line and make us all think they really care. They have fooled a lot of people and lined the pockets of our politicians so they must be good right?
There are some really good things about both the US and Canadian systems and some really bad. I wonder if there is a way to make this work to benefit patients and the providers who care for them while minimizing the bureaucratic and administrative costs? Then, how can we afford this for a country with 320 million people? Canada has 42 million and has its problems paying for it despite GST and higher average income tax and cost of living. Certainly worth an honest discussion.
Hello Mark and thanks for your thoughtful comments.
The good news is much of the change to reimbursement is focused on precisely that – paying for outcomes. Current CMS reimbursement methodology changes, bundled services, experiments with ACOs, all are intended to more closely link dollars to outcomes. The significant pay bump for Medicaid primary care services in 2014 and 2015 was another example.
We agree on the need to dump FFS and pay based on results. The path there is tricky indeed, but it’s a journey we must take. And we will screw up often on the way. That said, I’m really encouraged by some of the progress made my organizations such as CCA, where our ED diversion work has dramatically improved patient care and reduced expense.