AIG just increased reserves for workers’ comp claims in Florida by $109 million.
Attorneys reacted positively…
NCCI’s just-released analysis indicates this isn’t an anomaly; their experts estimate the unfunded liability may exceed $1 billion.
To give you some context, total workers’ comp premiums in the Sunshine state last year were $3.6 billion, making this potentially the largest unfunded liability ever seen.
Who’s affected
Insurance companies, self-insured employers including governmental entities, and employers with deductible plans.
What does this mean?
“Un-funded” means insurers won’t be able to increase premiums to cover the additional costs as those costs are for policy years that have expired and there is no mechanism to charge former policyholders higher premiums to recoup the losses. So, each employer and insurer has to come up with the funds.
Who benefits?
Attorneys. The additional funds will go to pay plaintiff and defense attorneys.
What caused this?
Three decisions by the Florida Supreme Court. Taken together, the decisions essentially overturn the limits on plaintiff attorney fees, allowing those attorneys to charge hourly fees instead of a percentage of their client’s benefits.
Previous reforms were motivated by high plaintiff legal costs as attorneys were paid their hourly rate regardless of the amount awarded to their client. This incentivized attorneys to litigate, as any work was compensated, regardless of the outcome. Taken to the extreme, claimant attorneys would spend hours litigating a denied office visit or X-Ray, racking up legal costs far above the actual cost of the denied service.
The reform sought to remove this incentive by paying attorneys a percentage of the actual award instead of an unlimited hourly-rate-based charge.
What does this mean for you?
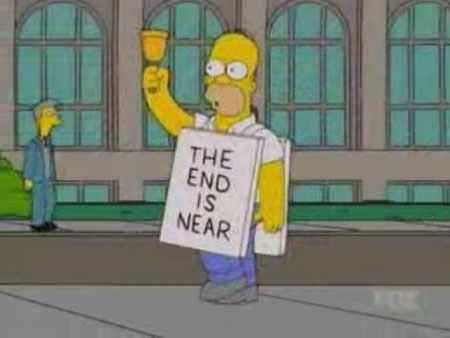
A totally miserable weekend – and many weeks to come – for Florida’s self-insured employers and insurers.
Party time for work comp attorneys.