Had a chance to sit down with WCRI CEO John Ruser a couple weeks ago and get his take on the Institute’s Annual Meeting, scheduled for March 22-23.
For those who have yet to attend WCRI, get yourself there this year…and unlike other conferences, attendance is limited.
I’d strongly encourage you to register now if you haven’t already…
MCM – What’s going to be different about this year’s conference?
JR – We are going to start with a focus on the future – Dr. Erica L. Groshen, former Commissioner of Labor Statistics and head of the U.S. Bureau of Labor Statistics will open with a discussion of the changing workforce and technology’s influence from the perspective of a labor economist, more about what is going to happen. The theme throughout the conference is we will revisit that. The Sedgwick Institute’s Dr. Rick Victor (former WCRI CEO) will speak to the challenges facing work comp system including the changes in the workforce, We will close with a panel discussion to hear from different perspectives on this theme.
MCM – Why this focus?
JR – There’s been an acceleration in the rate of change in the workforce, we thought it was time to bring that topic into the conference and bring it to bear on workers’ compensation in particular, it’s time to start considering this in our conference. I anticipate there will be discussion of potential impact of these changes on claim frequency and claim severity.
MCM – Any teasers you can provide on what those trends might look like?
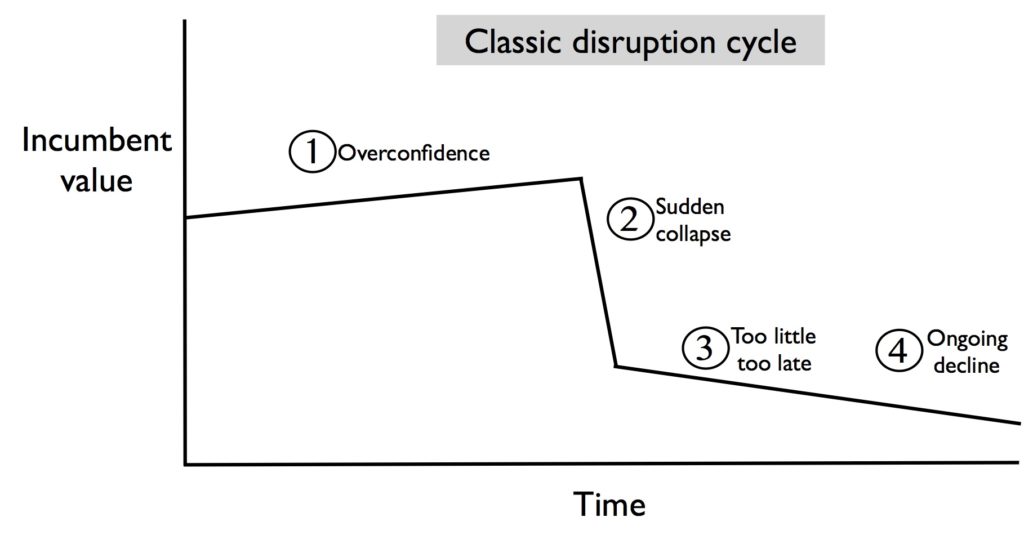
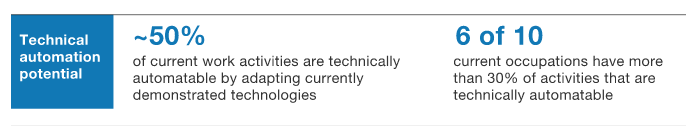
JR – In general, what’s going on in the economy in the labor market is the substitution of capital for labor; capital we used to think of as heavy machines, now it’s software and computers are driving the trend where high risk jobs will go away because of substitution of capital for labor.
Since I’m an optimist and this has been happening for 150 years or so, I believe new jobs will spring up, the question is what does that mean for workers’ comp. Along with that is the change in the employment relationship typified in part by Uber, but its gong to be amore general aspect of the labor market where workers won’t necessarily be attached to employers in the way they were before. That certainly creates challenges for workers’ compensation.
MCM – The implication is that insuring occupationally related injuries and illnesses is going to fundamentally change, is that fair?
JR – It certainly will change. We’ve seen a quarter-century of declines in OSHA reportables and claiming rates, there is a notion the workforce is changing so there aren’t as many claims as there were in the past.
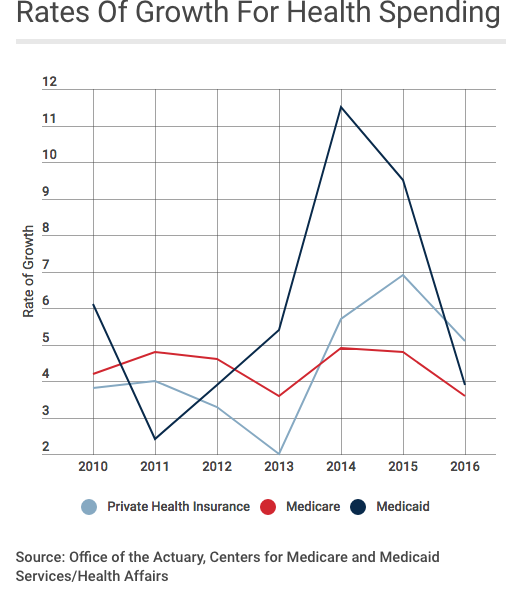
MCM – There is some indication that wages are heading up in some states, but given the substitution of capital for labor, that means folks in low wage jobs are not going to see increases in pay. For that and other reasons is it likely we will see medical expenses continue to increase as a percentage of claims?
JR – This is the area that Dr Groshen is going to get into…There are other factors as well, new technology that will help workers recover faster or even survive accidents that they wouldn’t have before. With that comes higher medical costs. Advanced prosthetics allow injured workers to function better, and while costs will go down over time, for now those devices are quite expensive.
MCM – Is there going to be discussion about Artificial Intelligence and the role that is going to play?
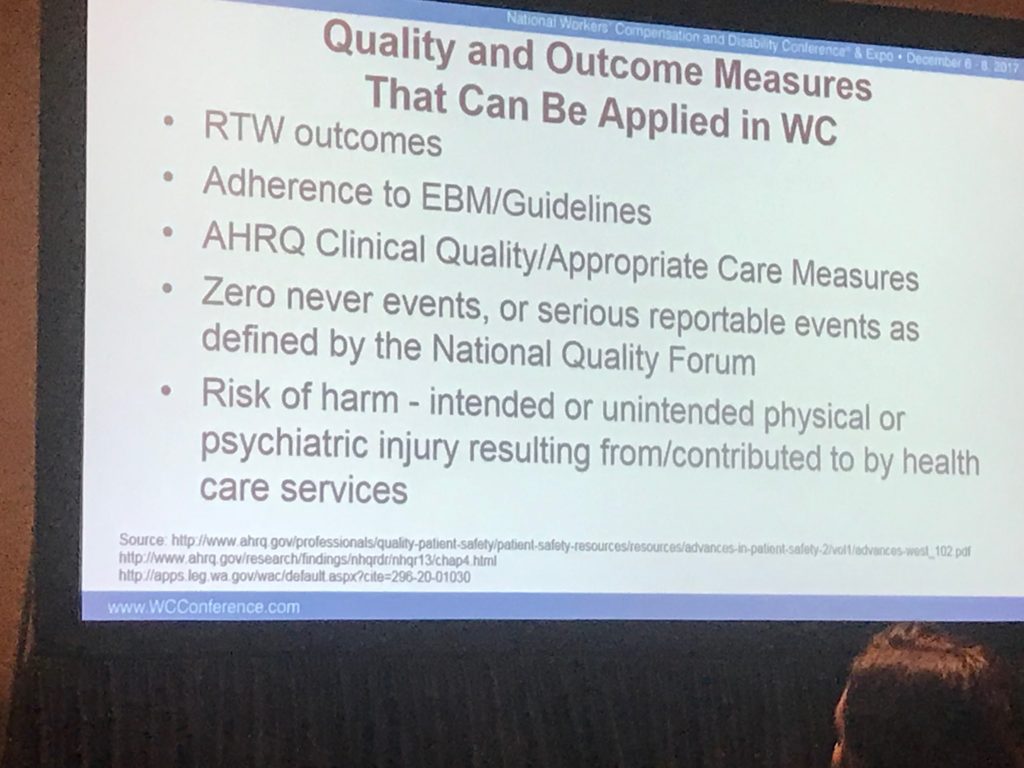
JR – Yes, that is likely to come up. There are lots of other topics, for example are we ready for value-based care? We are doing work interviewing stakeholders to determine if we are ready for that, and that will be a discussion topic at the conference. We have a session on opioids and the impact of opioids on return to work. The National Safety Council and a large employer will talk about the issue of opioids in the workplace.
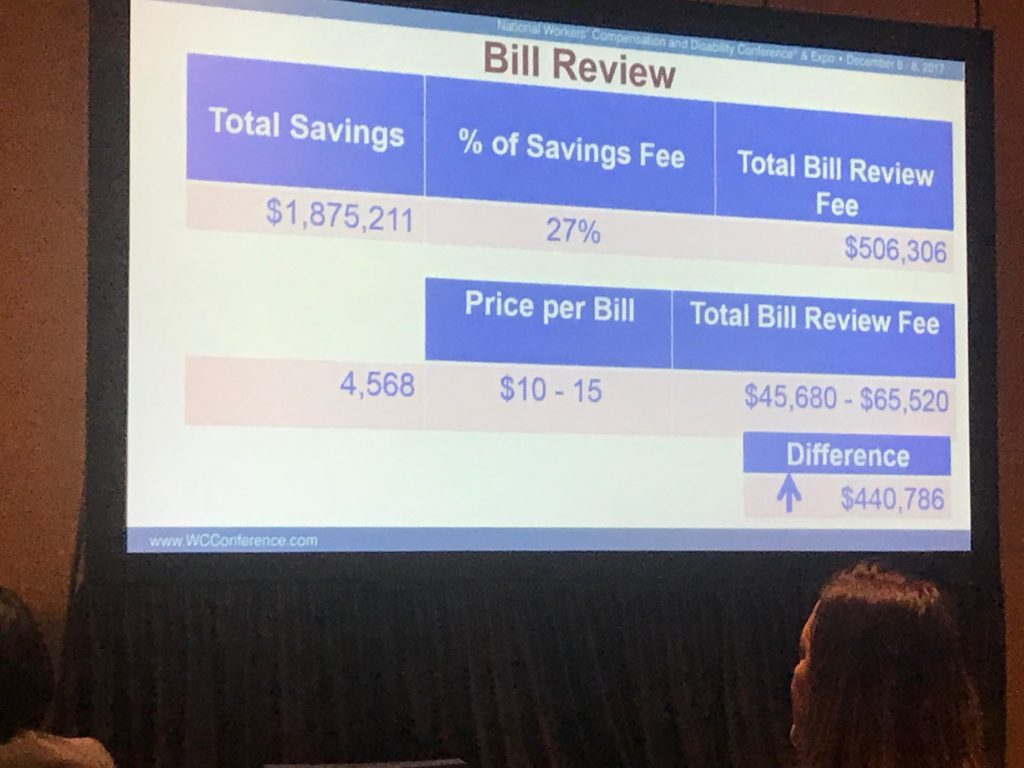
Fee schedules, prices, and access to care is always a topic of interest. We will be looking at this, in particular comparing group health to workers’ compensation in several areas including delays in accessing primary care and other types of treatment.
The agenda is here.
2019’s conference will be in Phoenix…