After my posts last week it is clear there’s a lot of misinformation and misunderstanding about the CDC’s opioid and chronic pain guidelines. At MCM we take the old-school approach to these things; we focus on the facts.
So, here they are.
The CDC’s guidelines mandate strict limits on dosage and require tapering for patients on long-term opioids.
False. As Dr Beth Darnall of Stanford University noted recently;
some health care organizations and states have wrongly cited the 2016 CDC Guideline as a basis to substantiate prescribing “dose-based limits” or to mandate that physicians and prescribers taper patients taking long-term opioids to specific thresholds (eg, < 90 mg, or < 50 mg). Such dose-based opioid prescribing policies are neither supported by the CDC, nor do they account for the medical circumstances of the individual patient. [emphasis added]
Further;
The CDC [issued] a clarifying statement that derided the misapplication of the opioid guideline and discouraged the dose-based policies and practices that fall outside of its scope, as well as use of the guideline to substantiate tapering.
The Guidelines for Prescribing Opioids for Chronic Pain were developed in secret.
False. The process fully complied with CDC and AHRQ requirements and standards, and the results were shared with the public and public comment sought prior to promulgation of the final guidelines in 2016.
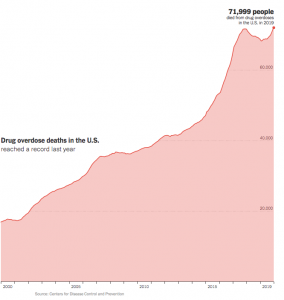
The Guidelines aren’t working; look at all the opioid-related deaths.
False.
- The big increase in drug poisonings (technical term for overdosing) is driven by a rapid increase in the use of synthetic opioids, both prescription and non-prescription. The synthetic opioid death rate increased over 1000% from 2013 to 2019, with the biggest increase in the western US. Fentanyl and Tramadol are examples of synthetic opioids
- There’s been a small but measurable decrease in the death rate (4.4 to 4.2) from prescription opioids that correlates with the guidelines’ publication date. Of course, correlation is not causation, but clearly the guidelines have been impactful.
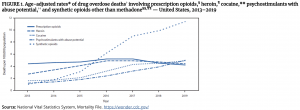
3. Further, when you count the deaths due solely to prescription opioids, the drop in the prescription opioid death rate is even more remarkable. The bold line is prescription opioid-only; the guidelines were introduced in 2016.
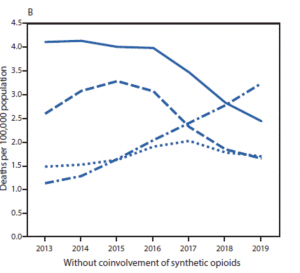
The net is those who claim the guidelines are somehow “failing” are conflating law enforcement issues with public health issues, and are ignoring the very real post-guideline decline in deaths from prescription opioids.
The guidelines are killing people.
The guidelines are just that – guidelines.
The guidelines do NOT require or mandate dosage restrictions or tapering. Blaming the guidelines – and those who developed the guidelines – for physicians not following the guideline’s explicit recommendations is wrong, and does nothing to solve the problem of bad legislation and poor physician behavior.
Here’s what the CDC actually said:
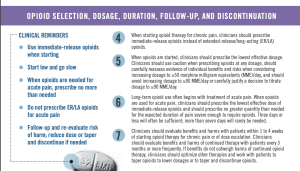
Clinicians should evaluate benefits and harms of continued therapy with patients every 3 months or more frequently. If benefits do not outweigh harms of continued opioid therapy, clinicians should optimize other therapies and work with patients to taper opioids to lower dosages or to taper and discontinue opioids. [emphasis added]
There are a lot of anecdotal reports of patients unable to get prescriptions renewed or otherwise forced off their opioid regimen, many with awful consequences. Yes, the guidelines did suggest/encourage/support these tools in certain circumstances, but – as you can read above – these are NOT requirements and require clinicians to evaluate and balance risk and harm.
What does this mean for you?
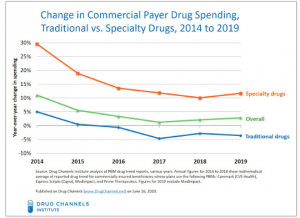
The real problem with Opioid Guidelines is states, insurers, and other entities – as well as prescribing physicians – failing to use the guidelines as intended.
reminder to commenters – valid email addresses are required, and disagreements are welcome as long as they are supported with credible citations.