We’re pushing to finish CompPharma’s Annual Survey of Prescription Drug Management in Workers’ Comp next week. After cleaning up the data, we’ve got final figures.
Quick takeaway – we workers comp types are doing a MUCH better job controlling drug usage than the rest of the world – and MUCH MUCH better controlling opioids.
Here are a few key data points:
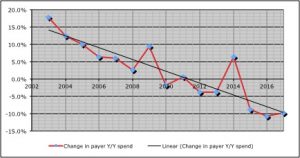
- Total drug spend was down almost 10 percent last year; drug costs are down 22 percent over the last six years
- In contrast, other payers’ spend dropped 2.1%.
- Opioid spend decreased by a third over the last two years.
- Other payers’ opioid spend dropped by less than half that – 14.9%.
While decreases in opioid spend have been dramatic, payers are still extremely concerned about opioid consumption – especially among long-term patients.
There’s a widespread and deep concern among respondents (29 payers of all types) that we’re a long way from figuring out how to help long-term opioid users reduce/eliminate their drug consumption.
This year we dug deep into that issue, and one key takeaway is the current regulatory focus on formularies and utilization review is focusing on a problem – initial prescriptions of opioids – that, while not solved, is much better controlled.
Where payers, patients, prescribers, and PBMs need regulatory help is with chronic opioid patients. Respondents had a raft of suggestions…
- mandatory urine drug testing done by labs not affiliated with the prescribing physician
- prescriber documentation of improvements in pain and functionality required before continuing dosing
- allow payers to reimburse for opioid recovery services while eliminating responsibility for non-opioid related psychological issues
What does this mean for you?
Work comp isn’t known as an innovative or progressive – yet here you are, well in front of other payers and work comp regulators.
Well done.



Joe – I can’t think of one area where the WC industry has truly partnered together to effect change like this. Thank you for helping lead the charge and raising awareness. Question for you: For those older claims , what solutions are you seeing in the marketplace that are truly helping people who have long-term dependence on opioids? BTW – Is that you in the Kayak?
Hi Brad – thanks for the comment. The entire industry deserves credit.
I’m digging into how specific payers have positively affected change among long time chronic opioid patients and will have that in the Survey report.
Quick point – one of the biggest obstacles appears to be fear of pain. Completely understandable; patients’ fear must be addressed before any solutions can begin.
That isn’t me in the kayak…I’m a flat water guy! https://www.healthstrategyassoc.com/paduda.html
Joe – it’s not just the fear of pain, it’s the actual pain which I never experienced until a recent sciatica problem shooting pain down my leg & numbing my toes. Still in treatment protocol which includes a limited amount of opioid which so far is the most effective pain relief. I limit the dosage to one at night to help me get to sleep. I’m trying non-opioid alternatives which so far get me through the day with a tolerable amount of pain. The experience has given me more perspective on the problem and the need to find better alternatives to opioids. BTY, I was wondering if that was Sandy in the kayak.
Thanks for this Bruce – great point and one I missed. Hope you are able to get relief.
I don’t think it was Sandy, but it could have been!
Just a question – and I do not know the answer, nor do I necessarily have a position: WC has seen great improvement in our opioid efforts, particularly as compared to others (presumably health plans). Could it be that we’ve seen those greater decreases, because we had fewer controls on prescriptions in the first place? I don’t know much about other health programs, but WC traditionally has had few, if any, controls on prescriptions – which lead to our recognition of the problem of uncontrolled opioid prescriptions in the first place. Health plans have had formularies for years; health plans have provider contracts by which providers must perform in certain ways; health plans have contracts by which they can deny treatments or prescriptions. Can our significant numbers decreases, again in comparison to other programs, be a reflection of laws and society changing to allow WC to apply similar controls ?
Peter – that is a very good question, and one I for which I too don’t have a clear answer. My guess is WC has been a soft target due to lack of ability to restrict inappropriate treatment of all kinds – including opioids. (see compounds, doc-dispensed drugs, spinal implants…)
That said, my sense is WC still doesn’t have near the degree of control governmental or private insurers do over formularies and prescribing.
So, we’re doing a lot with what we have, which isn’t near enough.
Agreed!