I’ve been thinking long and hard about why our health insurance and healthcare systems are such a clustermess. Hugely costly, lamentable outcomes, a morass of bureaucracy, red tape and stupid rules enriching a few and impoverishing many.
So, I think I have a solution – and it involves workers’ comp.
First, the problem.
Today I’m reprising a post from a couple years back – if anything it is more accurate today than it was way back then.
If you had “government” health insurance for the last decade, your costs would be 20 – 25% lower today.
That’s because private insurers have not controlled spending nearly as well as Medicare and Medicaid have. This from KFN via Axios.
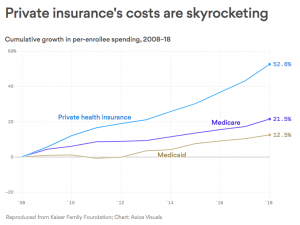
Doesn’t matter what your economic or political ideology is – that’s a fact.
You and your insurance company pay your doctors and hospital more than twice what Medicare does. Yes, the Feds can exert pricing power – but why can’t United Healthcare, or Aetna, or Blue Cross?
Those healthcare giants should be able to negotiate better deals with providers; they have massive buying power and millions of members to leverage. They should be able to use that power to give you lower insurance costs – but they can’t.
Those private insurers are (theoretically) more nimble, smarter, better run, and more efficient than the government. And they have hundreds of billions of healthcare dollars to leverage.
Yet they’ve failed to outperform a bunch of bureaucrats.
I won’t dive into the “whys” today, because that would take away from the over-arching truth – government has been much more effective than private insurers.
What does this mean for you?
Cutting your health insurance costs by a quarter = more dollars you could have spent on other stuff.
note – happy to hear other thoughts; please use citations to back up any assertions.



Definitively payers could do a better job of negotiating rates, however, the oligarchies and monopolies that are health systems that dominate far too many geographic regions demand higher reimbursements, and payers have little choice when a system owns the physicians, the hospital, and most of the ancillaries. Add to this that too often employers demand the inclusion of certain providers in a payers network if they are going to contract with an insurer.
Thanks for the note Robert.
As with any intermediary, payers’ job is to deliver the right solution at an affordable price. Reality is the big commercial payers directly benefit from those higher rates charged by health systems; higher prices = higher costs = higher premiums = higher stock prices.
That works until it doesn’t.
We are rapidly approaching the “it doesn’t” point.
Instead of lamenting the problems, UHC Aetna Centene et al would far better serve their customers if they figured out how to dis-intermediate those health systems. UHC is making some progress on this front – but its competitors are not.
Your point about employers is certainly valid; some are part of the problem. Others are getting smarter but they are few and far between.
be well Joe
Managed Care was developed to manage care. This is not happening. I have a friend who called her insurance company to talk to the case manager about a new diagnosis of cancer. She was told she was not sick enough for a case manager!
Anne – if you’re able, please identify the insurer.
Perhaps we can convince said insurer to perform a headectomy – defined as removing the head from the lower end of the gastrointestinal track.
be well – Joe
Nothing has even come close than my Medicare in providing quality medical treatment at sustainable costs. And no “Medicare Advantage” HMO or PPO plan! “Managed Care” in the health benefit system has become “Maximize Profits.” I see whatever provider I want whenever I want.
Joe you have taken on a big complicated topic here. I will keep my response simple and speak to my direct experience of working within this healthcare marketplace for 30 plus years. I can say the commercial payers do control rates in the world of the rehabilitation professions (PT, OT, SLP). They can do this because we are generally fragmented especially in the outpt world and have very little power to negotiate rates like the big health systems. We are also a very small part of the system in general. Employers usually do not advocate for their therapy providers. Just not on the radar.
The big health systems and their rehab departments get much higher reimbursement comparatively than us out in the private practice world. We are pretty much told by the commercial payers to take it or leave it. Our reimbursements from all the major commercials are sadly lower than what my plumber gets paid. And, around 50% of the Medicare Physician fee schedule.
I get the large commercials can’t or won’t play hardball with the large health systems because they need them for the foundations of their networks. These provider systems (that are consolidating more and more into larger and larger organization) have done this for this very reason. Buying power to combat what were dwindling reimbursements. This kind of consolidation is starting in the world or rehabilitation. I am not a fan of this corporate world of medicine or rehabilitation but it is a reaction to the broken system. We cannot survive in a world of dwindling reimbursements and rising costs. Not a good recipe for all the wonderful therapy providers out there helping keep America moving and productive.
I do not pretend to be an expert but I do have some experience and perspective. I am from Canada and have direct experience in their world of universal healthcare as both a provider and patient. Being in the US for 31 years has shown me the good and bad parts of a system built on capitalism and greed. There are really some very good parts of both types of systems (and plenty of bad). As you and some of the responders have mentioned the big payers have different motivations. It is called money and profits. And, they sure do have profits and executives making huge salaries and bonuses. The public is paying for their inefficiencies paying more in premiums and cost sharing and getting less coverage. Anyone paying for health insurance over the past 20 years will attest to this.
As you point out, things can be done better. Private companies can generally beat out a government run bureaucratic system any day of the week. But, not in this sector for reasons you bring to light. Why not a system where the payers are set up as non-profits but run by private entities? I think of the Red Cross or other such large organizations who run much more efficiently because Wall Street and profits are taken out of the equation. Just not sure our health as a nation is compatible with a system built on greed and profits. I will note I believe in capitalism. Just not sure my beloved capitalism can live in harmony with our health as a nation?
Thanks for the thoughtful note Mark.
Your description of the challenges faced by non-health system affiliated providers are spot on and reflect the power of the health system lobby and the perverse reimbursement mechanism that way overpays health-system affiliated providers.
This is just one more indication of the power and influence of the medical-industrial complex.
be well Joe