We’re pushing to finish CompPharma’s Annual Survey of Prescription Drug Management in Workers’ Comp next week. After cleaning up the data, we’ve got final figures.
Quick takeaway – we workers comp types are doing a MUCH better job controlling drug usage than the rest of the world – and MUCH MUCH better controlling opioids.
Here are a few key data points:
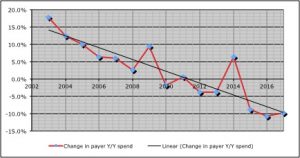
- Total drug spend was down almost 10 percent last year; drug costs are down 22 percent over the last six years
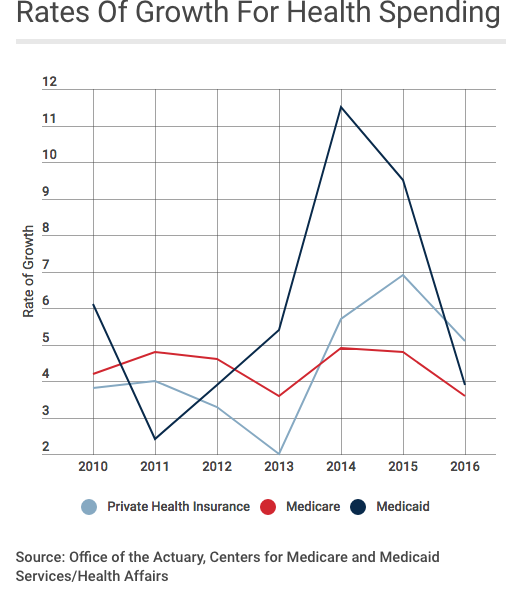
- In contrast, other payers’ spend dropped 2.1%.
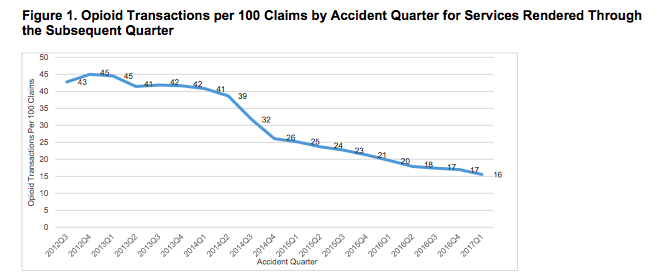
- Opioid spend decreased by a third over the last two years.
- Other payers’ opioid spend dropped by less than half that – 14.9%.
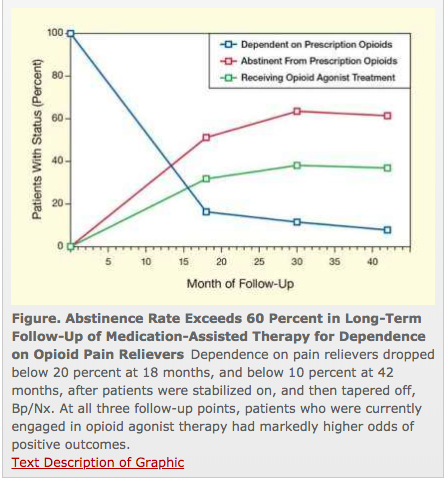
While decreases in opioid spend have been dramatic, payers are still extremely concerned about opioid consumption – especially among long-term patients.
There’s a widespread and deep concern among respondents (29 payers of all types) that we’re a long way from figuring out how to help long-term opioid users reduce/eliminate their drug consumption.
This year we dug deep into that issue, and one key takeaway is the current regulatory focus on formularies and utilization review is focusing on a problem – initial prescriptions of opioids – that, while not solved, is much better controlled.
Where payers, patients, prescribers, and PBMs need regulatory help is with chronic opioid patients. Respondents had a raft of suggestions…
- mandatory urine drug testing done by labs not affiliated with the prescribing physician
- prescriber documentation of improvements in pain and functionality required before continuing dosing
- allow payers to reimburse for opioid recovery services while eliminating responsibility for non-opioid related psychological issues
What does this mean for you?
Work comp isn’t known as an innovative or progressive – yet here you are, well in front of other payers and work comp regulators.
Well done.