Barry Lipton PhD did a quick review of a few ways work comp and group health differ – and how they are sometimes comparable.
The biggest difference is that workers’ comp is very focused on return to work, and more broadly, we care more about functionality. In group health, not so much.
Differences – other than the obvious e.g. WC=ortho and trauma; group health= everything
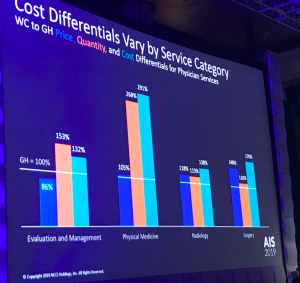
- price differences are 12% higher for work comp than group health,
- while utilization is 60% higher for workers’ comp
- so total costs are 77% higher.
This differs by state, with Alabama, Missouri, and Virginia showing the biggest cost difference compared to national averages, and Colorado and South Dakota with the lowest cost compared to that average.
It also differs by type of service – not surprisingly physical medicine is used much more in workers’ comp, driven almost entirely by more utilization.
That’s not surprising, as comp conditions are predominantly musculoskeletal injuries and focused on return to functionality, while group health deals with many more conditions and RTW is irrelevant.
There’s also a big difference in the cost of MRIs…
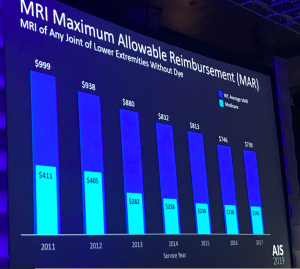
You can see that Medicare pays way less than work comp (WC is blue, Medicare is green-ish). You can also see the impact of Medicare’s change in reimbursement in 2013; it started to really impact workers comp in the years after 2014 as regulators adopted/factored in/used Medicare’s rate for reimbursement in their state.
What does this mean for you?
Price + Utilization = Cost. But one has to factor in RTW in comp, a focus that is nonexistent in group health.



As a nurse case manager, I see a few different things that differ between WC and traditional insurance. One is that the injured worker is ‘paid’ when injured. Even if it is only a portion of their salary, it is something and many times this turns into the reason why the IW does not go back to work. I agree the focus in WC is returning the injured worker to work and this is not as prominent in the group health world, but it is just as important. As a Certified Case Manager, it is my role to help the patient with traditional insurance to continue to work or they are at risk of losing their healthcare insurance. Once that happens, they are limited to their care. Also, unless they have a disability plan, they also lose their income which put a great strain on the ‘member’ and their family. As many in the industry have said if you have to get hurt or sick, make sure it is on WC as you have many more options. My role as a case manager is to make sure the patient (IW or member) receive the right care, at the right time, in the most cost-effective manner and in the least restrive setting. Everyone needs help to navigate the complex healthcare system. it is just too complex to go it alone regardless of the payer.
Hey Joe,
I agree that RTW and functionality are key issues in WC. You also correctly point out that provider WC fee schedules/rates tend to be much HIGHER than Medicare rates, which should make many providers happy.
But for Radiologists (think MRIs), Neurologists (think EMGs) and Physical Therapists (think PT and OT), many of their WC referrals come from provider scheduling networks that pay the provider BELOW Medicare rates.
I’d love to see more research on the impact of such low “wholesale” rates on RTW, total indemnity payments, litigation costs, and utilization numbers. Do you know of any such studies?
Hello Dick – thanks for the question.
In all the studies assessing reimbursement, quality of care, outcomes and the like, I’ve read, I’ve never seen one that showed a positive correlation between higher reimbursement and better outcomes.
Hey Joe,
I seem to remember a presentation last year, I think, at AIS by Alex Swerdlow that showed that MPNs in California that focused on provider discounts had significantly higher medical costs and indemnity costs compared to those that focused instead on quality. And the difference was very significant. Do you have a copy of that?
Dick – I do have a copy of that presentation. It’s easily found via the web. Not sure how you drew that conclusion from Alex’ presentation. I reviewed it again and couldn’t find anything that points to that result. You may be thinking about the discussion of “practice makes perfect” that built off CWCI’s seminal 2003 paper of the same name. However, that paper – and subsequent updates – didn’t produce the result you describe.
California is considering outlawing contracting below medicare fee schedule. While there are no studies I am certain that providers have learned who their partners are and where they can expect to be cheated.