Randy Lea MD of the Dartmouth Institute (one of the nation’s leading healthcare research organizations, and my personal favorite) just completed research on value-based care (VBC) in work comp – a timely and much-needed project. Dr Lea presented at last week’s WCRI Conference.
Here are my takeaways.
Spoiler alert – value-based care is not getting much traction – and I don’t think it will.
First, the research was more of a survey of what stakeholders want, expect, can do, and think is necessary to bring VBC than a detailed description of what actually exists today. In that way, it’s helpful as it indicates what factors may/will lead to more VBC in work comp.
As much as I respect the Dartmouth Institute and appreciate Dr Lea’s insights, I found the presentation hard to follow. There was just too much information crammed into too little time.
Stakeholder readiness
Providers – only one engaged in a WC VBC pilot program; many were prepared and waiting, but “there’s no opportunity for them to engage at this time.”
Payers – only one is doing VBC – and that is bundled payments. Payers were more focused on high-performing networks, not real VBC. Also doubt the model will be sustainable.
Regulators – again, only one doing VBS, that one has seen positive results, and is ready to expand. access, quality, and are coordination. Not much going on, but many are at least thinking about it.
Now into the meat – their thinking about how VBC might actually occur in workers’ comp.
Conditions that were popular for inclusion in a VBC model included spine, shoulder, knee, CTS, and co-morbidities plus the condition.
First, we need a regulatory environment that is favorable to VBC. No surprise here, although all recommended employer direction, mandated medical treatment guidelines, reduced fee schedules (?!), reduced UR.
Second, providers need enough patients.
Third, there was a lot of concern around RTW, causation, and impairment and who is involved and how decisions around those key issues will be made and on what basis.
Development guidelines
- Need a set of values that are shared by the stakeholders that guide development
- Rewards for good performing providers
- Transparency across all stakeholders
- Outcomes focused, not discount-driven
- Adaptability to current programs and regulatory conditions
- Fair and quick reimbursement of providers
- Reimbursement based on guidelines and compliance w MTG
- Eliminate fee schedules
- Need real steerage of patients
- Tight definition of outcomes is mandatory, need real specificity around things like RTW.
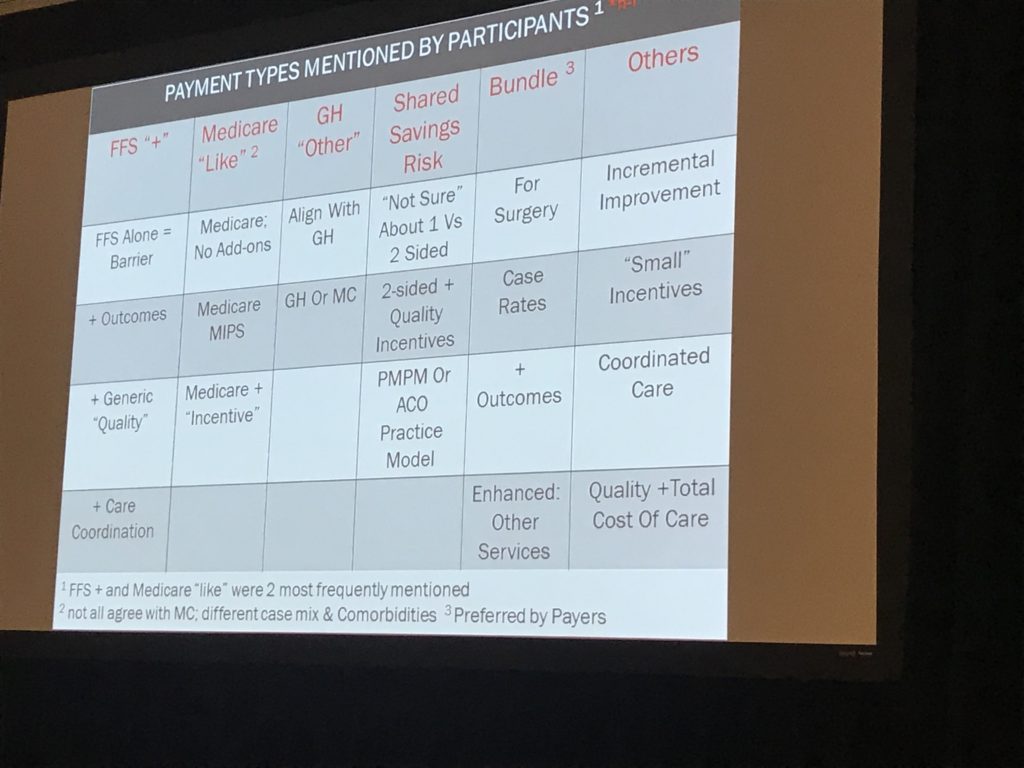
Payment types – participants reviewed a variety of types of reimbursement, with most payers looking for bundled payments – no surprise.
I also have to note that my main takeaway was this – work comp is a couple of decades behind the rest of the world – and it isn’t catching up. If anything, we’re falling further behind.
I say this because this is some pretty basic stuff compared to what we see in Medicaid or Medicare.
My view is there are any number of reasons VBC is not going to happen in WC.
- There are not enough cases; providers won’t be interested in risk-taking if there aren’t enough cases to spread the risk.
- Providers don’t have to take risk; in many states there’s no or limited employer direction, so no guarantee they’ll get a minimum number of cases.
- Litigation – providers may have to provide documentation and perhaps testify, something no one wants to risk.
- Payers are far too wedded to the percentage of savings profit machine.
What does this mean for you?
Bundled payments aren’t really value-based care. And even those are few and far between, for good reason.



Joe,
I agree that the complexities of the WC system, not the injuries, make the use of VBC challenging. You noted a number of those challenges in your post that make it difficult to move to a new model. The providers are not going to want to take risk without more control – why should they?
Perhaps there is a hybrid approach that could fit within the WC system. The question then becomes is it worth it?
The only model in WC that has some of the elements of VBC is the Paradigm approach to CAT cases. Obviously these are limited in number and very different than the average WC case but, they did come up with a model that sets the fees and tracks to outcomes during the various phases of the treatment. You would have to check with Paradigm on the acceptance rate for their Risk model which I am pretty sure is not every case.
There are still many out there, employers and carriers, that like the pay as you go approach. Cash is King and cashflow does play a part in the claim payment equation. Paying up front for care may not be the desired approach when you can pay it over time. I think people would be surprised at how often the cashflow factor comes into play in managing claims.
The alignment of stakeholder incentives produces better results at lower costs (medical and administrative expenses). If done right, can we at least agree that having VBC programs in WC would be a GOOD thing?
How we structure and manage provider compensation under VBC has almost always been the conundrum. Our entire system (read regulations and MC fees) is built upon a fee-for-service paradigm.
Maybe it isn’t value-based care that hasn’t worked. Rather, it is the all-or-nothing approach to value-based care that has been wrong. We should not give up on exploring new solutions to old problems.
I most certainly appreciate everyone’s comments and perspectives noted about VBC. The difficulty starts with the lack of an explicit standard roadmap to define what Value Based Care should be and how WC should move towards it.
There are many variables that define the equation, and depending upon the stakeholder’s prioritization of certain variables, the Value Output can vary markedly. For the moment, we can all acknowledge that VBC is much easier to discuss in theory and from a conceptual point of view. It’s less clear how to adopt and operationalize VBC in our industry. But as Les Shute noted in his comment, I definitely agree that barriers to VBC should not exclude or keep WC experts from “exploring new solutions to old problems.”
As Ken Martino mentioned in his comment, Paradigm Outcomes has been guaranteeing outcomes at a fixed cost for 25 years.
The growing fragmentation of our healthcare industry, as well as the misalignments in care perpetuated/enabled by a fee-for-service reimbursement system, actually reinforced the importance of the VBC approach embraced by Paradigm Outcomes in delivering a guaranteed outcome for a fixed cost at the onset of the catastrophic claim.
Although the future of VBC in WC is still uncertain, as to Joe’s prediction that VBC will not get much traction in WC — I definitely agree with Les that Paradigm’s results most certainly bolster and support the premise of “aligning all of the stakeholders incentives definitely produces better results at a lower costs.” Hence, I hope the leaders in WC industry will give it a chance.
Joe, thanks for the helpful overview from you and the commenters. An additional challenge, which I find really interesting when thinking about VBC in WC, is factoring in the impact of an injured worker’s ultimate indemnity status in establishing outcome parameters (Paradigm’s outcomes I recall, given the severity of the contracts they take on wouldn’t consider something like RTW for the most part). This speaks to aligning incentives for all stakeholders.
Good morning Joe. And yes, that was a load of information that I shared, but believe it or not, that was less than half of the material I could have included !! I think that is reflective of the magnitude of the larger conversation. Hopefully, in the foreseeable future we will find a way to present several of the more important themes in more detail. Best regards
Randall Lea
Randy – as one of the most respected experts in this field, your words carry much weight. Thanks for sharing with us.
Joe